گروه دارویی اکتوور
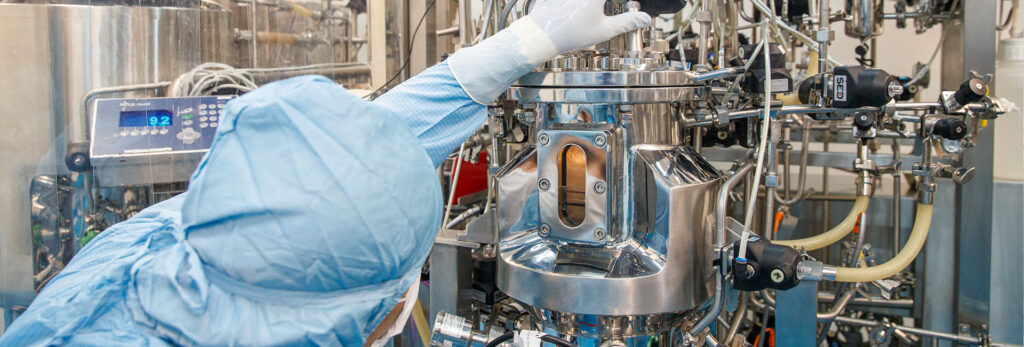
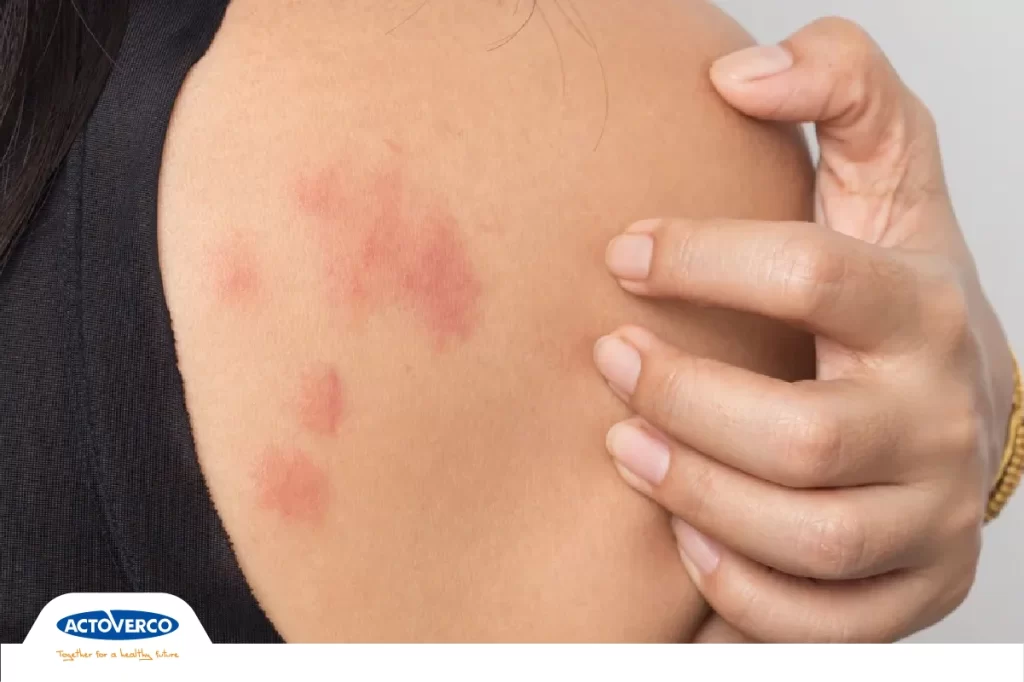
گروه دارویی اکتوور با بهکارگیری بیش از 2000 نفر از جوانان کارآمد کشور، در 15 حوزهی درمانی و با دارابودن بیش از 320 محصول دارویی، با لحاظ بالاترین استانداردهای مورد تایید سازمان های داخلی و بین المللی، تاکنون توانسته در تولید و تامین دارو با کسب افتخارات فراوان، بزرگترین و با سابقه ترین گروه خصوصی دارویی در ایران و خاورمیانه را تشکیل دهد. گروه دارویی اکتوور با هدف تولید و تأمین نیاز دارویی بیماران ایرانی در دستیابی به بهترین کیفیت، در رده جهانی، پایهگذاری شده است و همواره یکی از شرکت های پیشرو، در تولید بهترین داروهای بازار ایران و منطقه بوده است.